Home › Blog – Gladstones Private Rehab Clinic › Navigating the Intersection: ADHD, Developmental Trauma Disorder, and Substance Abuse in Youth
Teenagers, adolescents, and young adults under the age of 23 are particularly susceptible to addiction. Changing neurochemistry while going through puberty, increased pressure from peers and social groups, a still-growing understanding of the world and how it works, and the inability to deal with stress and pressure from parents, school, or early working life are all factors that might push a young person towards some sort of escapism.
These are all challenges that everyday, normal, and healthy teenagers and young people face.
But what about those who suffer from mental health disorders? What roles do ADHD and developmental trauma play in teenage substance abuse?
ADHD (Attention Deficit Hyperactivity Disorder) and DTD (Developmental Trauma Disorder, often referred to as childhood trauma) are both mental health disorders that can increase the risk factor for substance abuse in adolescents (Mariani and Levin and Carliner et al.). When risk evolves into addiction, both ADHD and DTD can further complicate rehab and treatment as they are often accompanied by co-occurring mental health disorders. These mental health disorders, developed due to increased stress and anxiety, must be considered alongside the challenges of dealing with physical dependency.
This article will take a closer look at the relationship between ADHD and DTD within the context of teenage addiction, breaking down where they overlap, how they contribute to an increased risk of substance abuse, and discussing prevention and treatment strategies.
ADHD is one of the most commonly diagnosed developmental disorders in children and teenagers, causing symptoms that make it difficult to be calm, focus, and concentrate on a single subject. Its causes are diverse and not fully understood, but could include genetics, prenatal exposure to substances, low birth weight, and brain injury. On the other hand, developmental trauma refers to chronic traumatic experiences during childhood, such as accidents, abuse, neglect, or the death of a loved one. DTD can lead to changes in brain circuitry, affecting mood and behaviour in the long run.
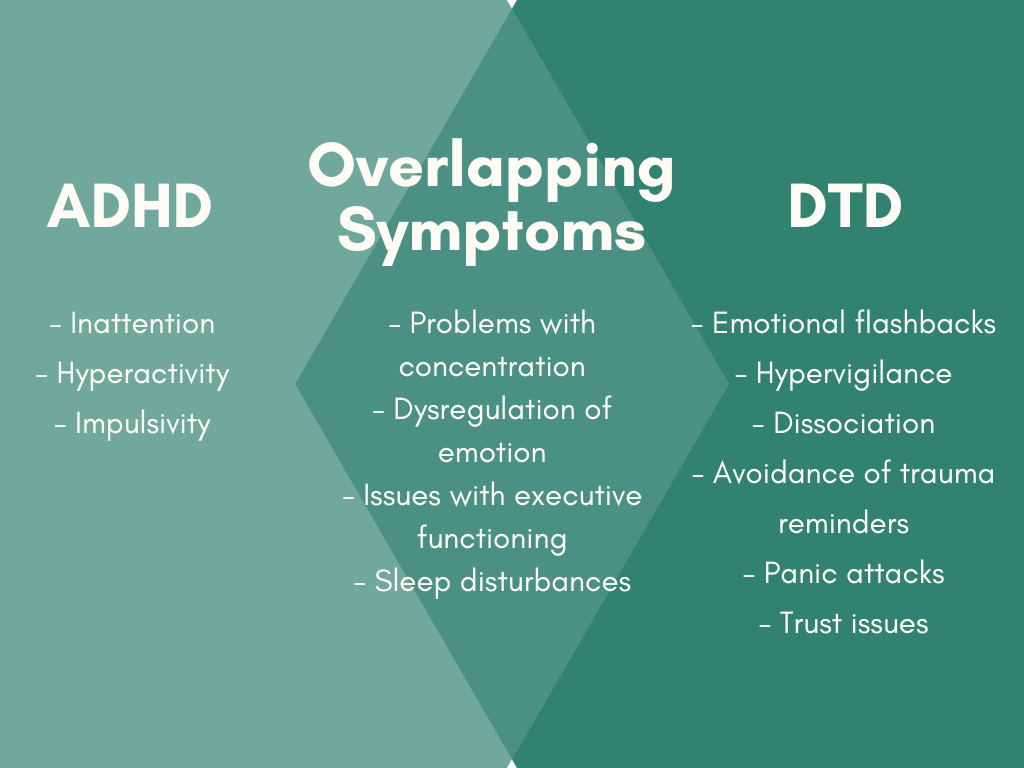
Despite being two completely distinct and separate mental health conditions, each with its own set of development factors, they do overlap significantly when it comes to their symptoms. This can easily complicate diagnosis and treatment. Looking at the image below, it’s not hard to see how a doctor might misdiagnose a 12-year-old presenting with a lack of concentration, poor emotional regulation, and regular sleep disturbances.
A misdiagnosis, especially one given at a younger age and never revisited, can lead to years of ineffective treatment that inadvertently causes more stress and anxiety, potentially even leading to the development of coexisting mental health disorders. Not seeing any improvement or changes in their condition, despite their best efforts, might cause a teen to believe that there is something wrong with them, something that nobody can fix, something to escape from through substances.
The link between ADHD and substance use disorder (SUD) is clear: more than 25% of adolescents seeking treatment for an SUD meet the diagnostic criteria for ADHD (Mariani and Levin).
What isn’t so clear is the link between the two. One theory that aims to explain the overlap between ADHD and the increased likelihood of developing a SUD attributes the higher co-occurrence rate to drugs emulating the effects of ADHD medication over the short term. Many ADHD medications are classified as CNS (central nervous system) stimulants and fall into the same classification as amphetamines.
When those suffering from diagnosed or undiagnosed ADHD take stimulant-class drugs such as amphetamines, cocaine, or MDMA, they might briefly feel a brief sense of clarity or relief from a scattered mind and attention. Ignoring this relief, along with the high from the drugs, can be incredibly difficult for adolescents who have never experienced a clear and focused mind before, almost certainly leading to further experimentation. If left unchecked or undiscovered, this self-medicating drug use will soon negate any ‘positive’ effects as the body develops a tolerance, doses start increasing, and the dark side of drug abuse starts rearing its head.
For a more detailed exploration of the complex link between ADHD and substance use disorder, including statistics, causes of ADHD, and the mechanisms of addiction, please read our article on ADHD and Substance Misuse.
DTD, not to be confused with PTSD which is typically the result of a single traumatic experience, stems from chronic and multifaceted negative experiences during childhood, often including mistreatment, abuse, violence, sexual harassment, and/or neglect. These experiences, especially at a young age, can lead to profound psychological and neurological changes in the brain, disrupting normal social and behavioural development.
The human brain is hard-wired to perform specific functions in different parts of the brain. It is thought that recurring trauma experienced during early development affects the parts of the brain associated with both survival and learning, ‘amplifying’ survival mechanisms such as hypervigilance, anticipation of harm, and protecting against damage caused by potential dangers at the cost of learning and development (Hodas).
Chronic stress at a young age can also lead to other normal brain and neurochemical development disruptions. Constantly elevated cortisol (the primary stress hormone) affects how a brain forms connections, leading to ‘use-dependent synaptic pruning’ (Australian Institute of Family Studies). Under chronic stress, the natural and healthy process of synaptic pruning leads to unwanted outcomes in which unhealthy pathways are strengthened at the expense of healthy ones.
As a pre-pubescent child grows up and goes through puberty, poorly developed interpersonal and emotional regulation skills, along with a brain that has suffered physical growth impairment, can easily lead to mental health disorders such as anxiety, depression, personality disorders, and more (Attachment & Trauma Network). All of these disorders are associated with an increased risk of developing a substance addiction.
While both ADHD and DTD can significantly increase the odds that a child will develop substance abuse issues as either a teenager or adult, an accurate and early diagnosis, active prevention measures, and early intervention if abuse is suspected, can significantly reduce the odds of full-blown substance addiction.
The first step in preventing harm is identifying the danger; however, in the case of complex mental health disorders, this is easier said than done. While we’ve already discussed how ADHD and DTD have a significant overlap in symptoms that could lead to a misdiagnosis, children at risk of developing DTD due to abuse, neglect, or an otherwise broken home face the additional challenge of likely never making it to a child welfare specialist or psychologist capable of diagnosing their condition. In some cases, their first experience with someone concerned about their long-term mental health and wellness might only come after an arrest or medical emergency, at which time a SUD may have already laid down roots.
Assuming that a child has the privilege of an early diagnosis of their condition, a combination of behavioural therapies and medication could make all the difference. A 2003 meta-analysis of the relationship between stimulant therapy and subsequent SUD in youths with ADHD showed that youths treated with prescribed stimulants had a 1.9-fold reduction in the risk of developing an SUD later in life (Wilens et al.); however, it must be noted that behavioural therapy for ADHD is much more commonplace than medication.
Except for medication used to treat co-occurring mental health disorders that developed as a direct result of childhood trauma, there aren’t any medications that would potentially help prevent the development of an SUD in adolescents suffering from DTD. At-risk children and teenagers’ best chance at a healthy and addiction-free life hinges on access to mental health services, trauma-informed care, substance abuse education, and, most importantly, strong and positive support from family members, peers, and other relationships. These protective factors can offer a buffer against the effects of trauma and provide a supportive environment for personal growth and development.
Attachment & Trauma Network. “Developmental Trauma Disorder | DTD vs. PTSD and CPTSD.” Attachment and Trauma Network, Attachment & Trauma Network, Inc., https://www.attachmenttraumanetwork.org/developmental-trauma-disorder/. Accessed 4 April 2024.
Australian Institute of Family Studies. “The effect of trauma on the brain development of children.” Australian Institute of Family Studies, Australian Institute of Family Studies, June 2016, https://aifs.gov.au/resources/practice-guides/effect-trauma-brain-development-children. Accessed 4 April 2024.
Carliner, H., et al. “Childhood Trauma and Illicit Drug Use in Adolescence: A Population-Based National Comorbidity Survey Replication–Adolescent Supplement Study.” Journal of the American Academy of Child & Adolescent Psychiatry, ScienceDirect, 9 November 2017, https://www.sciencedirect.com/science/article/abs/pii/S089085671630212X. Accessed 3 April 2024.
GOV.UK. “From harm to hope: A 10-year drugs plan to cut crime and save lives.” GOV.UK, GOV.UK, 6 December 2021, https://www.gov.uk/government/publications/from-harm-to-hope-a-10-year-drugs-plan-to-cut-crime-and-save-lives. Accessed 5 April 2024.
Hodas, Gordon R. “Trauma-informed services and trauma-specific care for Indigenous Australian children (resource sheet; 8 January 2014 edition)(AI.” Australian Institute of Health and Welfare, Australian Institute of Health and Welfare, 8 January 2014, https://www.aihw.gov.au/getmedia/e322914f-ac63-44f1-8c2f-4d84938fcd41/ctg-rs21.pdf.aspx?inline=true. Accessed 4 April 2024.
Mariani, John J., and Frances R. Levin. “Treatment Strategies for Co-Occurring ADHD and Substance Use Disorders.” NCBI, PubMed Central, 4 May 2009, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2676785/. Accessed 3 April 2024.
Wilens, T. E., et al. “Does stimulant therapy of attention-deficit/hyperactivity disorder beget later substance abuse? A meta-analytic review of the literature.” PubMed, National Library of Medicine, Jan 2003, https://pubmed.ncbi.nlm.nih.gov/12509574/. Accessed 4 April 2024.




With over 15 years experience our integrated approach to treating Mental Health & Addictions has transformed the lives of hundreds of people by empowering and supporting them to take back control of their lives.
GLADSTONES CLINIC LIMITED
The Wyastone Business Park
Wyastone Leys, Ganarew
Monmouth, NP25 3SR
Gladstones Clinic Cotswolds
Narles Farm, Dursley Road
Cambridge
Gloucestershire
GL2 7AB
Tel: 01453 890184
Gladstones Clinic London
64 Waverley Gardens
London
NW10 7EE
Tel: 020 8964 8516
Gladstones Clinic Bristol
48 St Paul’s Road
Clifton
Bristol
BS8 1LP
Tel: 0117 925 2995
Gladstones Clinic Cornwall
66 Lemon Street
Truro
Cornwall
TR1 2PN
Tel: 0117 925 2995
Copyright 2025 Gladstones Clinic – All Rights Reserved | Privacy Policy | Privacy Settings | Company Number: 07607877
If you would like to request a callback from our support team, please fill out the form below and we’ll get in touch with you as soon as possible.
