Enquire now
For a confidential chat call Freephone on 0808 258 2350
Home › Blog – Gladstones Private Rehab Clinic › The relationship between trauma and addiction: A layman’s guide
Trauma, a response to deeply distressing or disturbing events that overwhelm an individual’s ability to cope, can have a profound effect on one’s psychological well-being. It influences thoughts, behaviours, and emotions significantly and has been linked to a host of mental health disorders and substance addiction, both of which can severely affect one’s ability to live a healthy and fulfilling life.
Although psychologists and other specialists are continuously learning more about exactly what trauma does to our brains, trauma and its effects aren’t new to us. For as long as humans have been around, we’ve fought in wars, navigated natural disasters, dealt with the deaths of loved ones, and collectively experienced hundreds of millions of traumatic events.
Determining the exact moment we started using substances to treat trauma is impossible; however, the Ebers papyrus, an Egyptian medical papyrus dating back to roughly 1550 BC, makes specific mention of both opium and cannabis within the context of “calming the nerves” (drugtimeline.ca). Although not explicitly documented, it’s also very likely that traumatised soldiers returning from wars and crusades throughout history turned to alcohol or other substances available at the time to help deal with their reality.
While the term Post-Traumatic Stress Disorder (PTSD) wouldn’t be coined until decades later, soldiers returning home from the American Civil War (1861-1865) often suffered from what was referred to as “soldier’s heart” or “nostalgia”. Many of these soldiers turned to opium or heroin (both of which were legal and available at the time), with Horace B. Day writing in 1868 that “diseased and disabled soldiers released from hostile prisons, anguished and hopeless wives and mothers, made so by the slaughter of those who were dearest to them, have found, many of them, temporary relief from their sufferings in opium.” (Carroll)
As our modern understanding of psychology developed during the 20th century, especially after the world wars, a myriad of well-documented cases of “shell-shocked” and “combat fatigued” soldiers self-medicating with drugs and alcohol were recorded, establishing for the first time concrete evidence of the intersection between trauma, substance abuse, and addiction.
Today, psychiatrists around the world are acutely aware of how trauma, whether in the form of unexpected loss, violence, abuse, or any other form, can be a significant driving force in the development of substance addiction. Although there are no long-term benefits to self-medicating trauma with drugs or alcohol, their short-term effects do bring some relief, leading many down a path of further despair and darkness as addiction takes ever more control of their thoughts and lives.
Enquire now
The relationship between trauma and addiction goes well beyond just cause and effect. Their intersection is complex, nuanced, bidirectional, and influenced by a confluence of personal and biological factors. While this is a gross oversimplification of a highly complex phenomenon, comparing the differences between brains exposed to and unexposed to trauma is a good place to start.
In the untraumatized brain, cortisol (the stress hormone) is released to elevate blood sugar levels and increase glucose absorption in the brain when we are in crisis or danger. This is linked to the fight-or-flight response, increasing physical and mental performance when we need it most. While this is great news in the face of an imminent threat, prolonged elevated levels of cortisol are linked to various health concerns, including depression, anxiety, PTSD, and cardiovascular disease (Khoddam).
Brains affected by trauma have a difficult time shutting off cortisol production, even after the immediate threat or danger has passed. This leads to a constant cortisol overload, leaving one nearly permanently on edge, causing swings between hyperalertness and fatigued states, and increasing the likelihood of developing any of the mental health disorders mentioned above.
It’s important to understand that trauma impacts more than just the stress hormone in our bodies. When someone experiences trauma, it doesn’t only throw off the balance of cortisol; it affects the entire brain. This includes how the brain’s control centre (the frontal cortex) functions, affecting how we think and make decisions. It also influences the brain’s emotional hub, the amygdala, which can lead to heightened emotions and anxiety (Sherin and Nemeroff). These changes can reduce the activity in the parts of the brain responsible for memory and learning (like the hippocampus) and disrupt the balance of neurochemicals that keep our mood and reactions steady (Zhu et al.). While the sum of these changes doesn’t directly lead to substance abuse or addiction, they significantly increase the odds of developing mental health disorders that are strongly associated with drug and alcohol misuse.
Understanding the link between mental health disorders and the development of a substance addiction is much easier than understanding the link between trauma and mental health disorders.
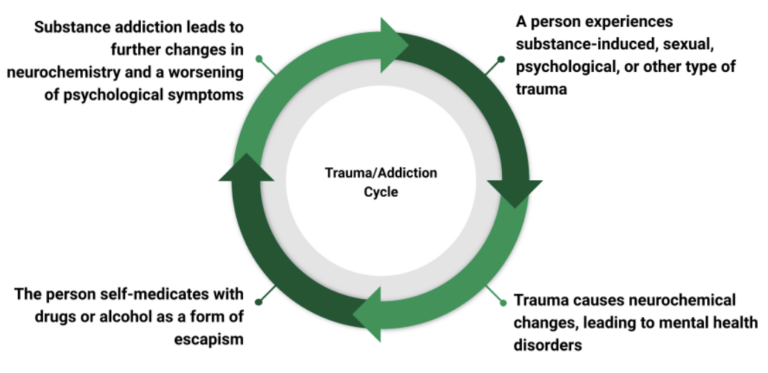
Anxiety disorders, depression, PTSD, and many other mental health disorders can do significant damage to one’s quality of life. They can cause one to experience constant anxiety over minor or even non-existent issues, fatigue, harm personal and social relationships, affect one’s ability to perform at work or meet responsibilities, and even lead to suicidal thoughts and behaviour. In the face of these challenges, substances like drugs or alcohol might seem like a reasonable, albeit short-lived, escape from an unbearable reality. This sort of self-medication, however, does more harm than good, as temporary relief quickly turns to dependency and full-blown substance addiction.
Over time, the cumulative harmful effects of substance abuse build up, causing both physical harm and worsening the psychological effects of the underlying mental health disorders. Conditions such as impaired memory and cognitive ability and reduced neurotransmitter activity due to substance abuse further compound stress and anxiety, leading to further trauma and the need for intervention.
Understanding the relationship between trauma and addiction is critical for the development of strategies and therapies that simultaneously address the underpinning trauma, physical substance addiction as a result of the trauma, and the new trauma caused by substance addiction.
For more than 20 years, Gladstones Clinic has been at the forefront of treating trauma, substance addiction, and mental health disorders. Our highly experienced team of psychologists, addiction specialists, and recovery workers takes a holistic and integrative approach to therapy and recovery, ensuring that all aspects of your condition(s) are acknowledged, understood, and addressed.
We offer specialised and personalised therapy, including trauma-informed care and dual diagnosis treatment, in a peaceful and comfortable residential setting where you can focus on recovery and reclaiming your life from the torment of trauma and substance abuse. After checking in with us, you can expect kind and compassionate care for the duration of your stay, as well as 24/7 medical supervision during detox that allows you to transition to primary care as seamlessly and comfortably as possible.
We employ a wide range of evidence-backed treatment modalities built around your unique situation and set of circumstances. While the exact treatment schedule is unique to each patient, those in dual-diagnosis treatment for trauma and addiction can typically expect a combination of Trauma-Focused Cognitive Behavioural Therapy (CBT), Dialectical Behaviour Therapy (DBT), group therapies, and holistic therapies for ‘whole-person’ recovery.
If you or a loved one is struggling with trauma-induced addiction, please contact Gladstones Clinic today for an obligation-free discussion of our treatment programmes, facilities, and treatment options available to you.
With Gladstones as your recovery partner, you’ll never be alone in the fight against trauma or addiction again.
If you or a loved one find yourself dealing with substance addiction or mental health disorders, we encourage you to contact us for a confidential, straightforward, and obligation-free conversation about all the treatment options available to you.
Carroll, Dillon J. “Civil War Veterans and Opiate Addiction in the Gilded Age.” The Journal of the Civil War Era, The Journal of the Civil War Era, 22 November 2016, https://www.journalofthecivilwarera.org/2016/11/civil-war-veterans-opiate-addiction-gilded-age/. Accessed 2 February 2024.
drugtimeline.ca. “Opium and cannabis mentioned in ancient Egyptian medical texts.” Opium and cannabis mentioned in ancient Egyptian medical texts, Drugtimeline.ca, https://drugtimeline.ca/event/opium-listed-natural-remedy-papyrus-ebers/. Accessed 2 Feb 2024.
Khoddam, Rubin. “How Trauma Affects the Body.” Psychology Today, Psychology Today, 3 March 2021, https://www.psychologytoday.com/us/blog/the-addiction-connection/202103/how-trauma-affects-the-body. Accessed 5 February 2024.
Sherin, J. E., and C. B. Nemeroff. “Post-traumatic stress disorder: the neurobiological impact of psychological trauma.” Dialogues Clin Neurosci., vol. 13, no. 3, 2011, pp. 263-278. National Library of Medicine, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3182008/. Accessed 2 Feb 2024.
Zhu, Xi, et al. “Researchers reveal how trauma changes the brain.” University of Rochester Medical Center, University of Rochester Medical Center, 7 December 2022, https://www.urmc.rochester.edu/news/publications/neuroscience/researchers-reveal-how-trauma-changes-the-brain. Accessed 8 February 2024.




With over 15 years experience our integrated approach to treating Mental Health & Addictions has transformed the lives of hundreds of people by empowering and supporting them to take back control of their lives.
GLADSTONES CLINIC LIMITED
The Wyastone Business Park
Wyastone Leys, Ganarew
Monmouth, NP25 3SR
Gladstones Clinic Cotswolds
Narles Farm, Dursley Road
Cambridge
Gloucestershire
GL2 7AB
Tel: 01453 890184
Gladstones Clinic London
64 Waverley Gardens
London
NW10 7EE
Tel: 020 8964 8516
Gladstones Clinic Bristol
48 St Paul’s Road
Clifton
Bristol
BS8 1LP
Tel: 0117 925 2995
Gladstones Clinic Cornwall
66 Lemon Street
Truro
Cornwall
TR1 2PN
Tel: 0117 925 2995
Copyright 2024 Gladstones Clinic – All Rights Reserved | Privacy Policy | Privacy Settings
